kottke.org posts about Ed Yong
Hey, everyone. I just wanted to update you on what’s been happening here at KDO HQ. As you might have noticed (and if my inbox is any indication, you have), I have pivoted to posting almost exclusively about the coup happening in the United States right now. My focus will be on this crisis for the foreseeable future. I don’t yet know to what extent other things will make it back into the mix. I still very much believe that we need art and beauty and laughter and distraction and all of that, but I also believe very strongly that this situation is too important and potentially dangerous to ignore. And it is largely being ignored by a mainstream press that has been softened up by years of conservative pushback, financial pressures, and hollowing out by Facebook & Google. But I have an independent website and a platform, and I’m going to use it the way that I have always used it: to inform people about the truth of the world (as best as I understand it) and what I feel is important.
I have pivoted like this a couple of times before: in the aftermath of 9/11 and during the pandemic. This situation feels as urgent now as those events did then. Witnessing the events of this past weekend, I felt very much like I did back in March 2020, before things shut down here in the US — you could see this huge tidal wave coming and everyone was still out on the beach sunbathing because the media and our elected officials weren’t meeting the moment. I believe that if this coup is allowed to continue and succeed, it will completely alter the course of American history — so I feel like I have no choice but to talk about it.
If you need to check out, I totally understand. I’ve heard from many readers over the years that some of you come to the site for a break from the horrible news of the world, and I know this pivot goes against that. I expect I will lose some readers and members over this — the membership page is right here if you’d like to change your status. For those who choose to continue to support the site, no matter what, my deep thanks and appreciation to you.
I’ll end on a personal note. I’ve talked a little about the impact that covering the pandemic for two years had on me, particularly in this post about Ed Yong’s talk at XOXO:
It was hard to hear about how his work “completely broke” him. To say that Yong’s experience mirrored my own is, according to the mild PTSD I’m experiencing as I consider everything he related in that video, an understatement. We covered the pandemic in different ways, but like Yong, I was completely consumed by it. I read hundreds(/thousands?) of stories, papers, and posts a week for more than a year, wrote hundreds of posts, and posted hundreds of links, trying to make sense of what was happening so that, hopefully, I could help others do the same. The sense of purpose and duty I felt to my readers — and to reality — was intense, to the point of overwhelm.
Like Yong, I eventually had to step back, taking a seven-month sabbatical in 2022. I didn’t talk about the pandemic at all in that post, but in retrospect, it was the catalyst for my break. Unlike Yong, I am back at it: hopefully more aware of my limits, running like it’s an ultramarathon rather than a sprint, trying to keep my empathy for others in the right frame so I can share their stories effectively without losing myself.
Covering the pandemic broke me. I spent the weekend and most of Monday wrestling with myself and asking, “Do you really want to put yourself through that again?” I could easily just go on posting like this existential threat to the United States isn’t happening. Like I said before, I believe we need — like they are actually necessary for life — art and beauty and laughter and distraction…and continuing to cover them would be a noble and respectable undertaking. But I eventually realized, thanks in part ot an intense session with my therapist on Tuesday, that in order to be true to myself, I need to do this.
Thankfully, I am in a much better place, mental health-wise, than I was 5 years ago. I know myself better and know how to take care of myself when I am professionally stressed out. There may be times when I need to step away and I thank you for your patience in advance. I hope that you’re doing whatever it is you need to do to take yourselves. 💞
Regarding comments: I haven’t been turning them on for any of the posts about the coup. I am trying to figure out how to turn them back on and not have the discussions mirror the sorts of unhelpful patterns that social media has conditioned us into following when discussing political issues online. I have turned them on for this post, but would encourage you to reflect on kottke.org’s community guidelines if you choose to participate; the short version: “be kind, generous, & constructive, bring facts, and try to leave the place better than you found it”. Thanks.
My favorite presentation at XOXO this year was Ed Yong’s talk about the pandemic, journalism, his work over the past four years, and the personal toll that all those things took on him. I just watched the entire thing again, riveted the whole time.
Hearing how thoughtfully & compassionately he approached his work during the pandemic was really inspirational: “My pillars are empathy, curiosity, and kindness — and much else flows from that.” And his defense of journalism, especially journalism as “a caretaking profession”:
For people who feel lost and alone, we get to say through our work: you are not. For people who feel like society has abandoned them and their lives do not matter, we get to say: actually, they fucking do. We are one of the only professions that can do that through our work and that can do that at scale — a scale commensurate with many of the crises that we face.
Then, it was hard to hear about how his work “completely broke” him. To say that Yong’s experience mirrored my own is, according to the mild PTSD I’m experiencing as I consider everything he related in that video, an understatement. We covered the pandemic in different ways, but like Yong, I was completely consumed by it. I read hundreds(/thousands?) of stories, papers, and posts a week for more than a year, wrote hundreds of posts, and posted hundreds of links, trying to make sense of what was happening so that, hopefully, I could help others do the same. The sense of purpose and duty I felt to my readers — and to reality — was intense, to the point of overwhelm.
Like Yong, I eventually had to step back, taking a seven-month sabbatical in 2022. I didn’t talk about the pandemic at all in that post, but in retrospect, it was the catalyst for my break. Unlike Yong, I am back at it: hopefully more aware of my limits, running like it’s an ultramarathon rather than a sprint, trying to keep my empathy for others in the right frame so I can share their stories effectively without losing myself.1
I didn’t get a chance to meet Yong in person at XOXO, so: Ed, thank you so much for all of your marvelous work and amazing talk and for setting an example of how to do compassionate, important work without compromising your values. (And I love seeing your bird photos pop up on Bluesky.)
In his newest piece for The Atlantic, Ed Yong explores why, despite more than 6 million official deaths worldwide and almost a million official deaths in the US, the toll of the pandemic isn’t provoking a massive social reckoning. This is a hell of an opening paragraph:
The United States reported more deaths from COVID-19 last Friday than deaths from Hurricane Katrina, more on any two recent weekdays than deaths during the 9/11 terrorist attacks, more last month than deaths from flu in a bad season, and more in two years than deaths from HIV during the four decades of the AIDS epidemic. At least 953,000 Americans have died from COVID, and the true toll is likely even higher because many deaths went uncounted. COVID is now the third leading cause of death in the U.S., after only heart disease and cancer, which are both catchall terms for many distinct diseases. The sheer scale of the tragedy strains the moral imagination. On May 24, 2020, as the United States passed 100,000 recorded deaths, The New York Times filled its front page with the names of the dead, describing their loss as “incalculable.” Now the nation hurtles toward a milestone of 1 million. What is 10 times incalculable?
And it just keeps going from there — this is one of those articles so well written and packed with so much information and insight that it’s difficult not to quote the whole thing, even though it paints a bleak picture of America. Read the whole thing here. See also Yong’s accompanying Twitter thread.
For The Atlantic, Ed Yong writes about an idea that has gained a certain amount of traction in recent weeks as hospital systems have been overwhelmed by the Omicron surge: medical care for unvaccinated people should be limited. Yong says that’s a very bad idea:
I ran this argument past several ethicists, clinicians, and public-health practitioners. Many of them sympathized with the exasperation and fear behind the sentiment. But all of them said that it was an awful idea — unethical, impractical, and founded on a shallow understanding of why some people remain unvaccinated.
“It’s an understandable response out of frustration and anger, and it is completely contrary to the tenets of medical ethics, which have stood pretty firm since the Second World War,” Matt Wynia, a doctor and ethicist at the University of Colorado, told me. “We don’t use the medical-care system as a way of meting out justice. We don’t use it to punish people for their social choices.” The matter “is pretty cut-and-dry,” Sara Murray, a hospitalist at UC San Francisco, added. “We have an ethical obligation to provide care for people regardless of the choices they made, and that stands true for our unvaccinated patients.”
Unvaccinated people are unvaccinated for a wide variety of reasons, many of them structural constraints beyond their control. Yong connects the care of the unvaccinated to the difficulty in receiving quality care already faced by women, Black people, and disabled people:
As health-care workers become more exhausted, demoralized, and furious, they might also unconsciously put less effort into treating unvaccinated patients. After all, implicit biases mean that many groups of people already receive poorer care despite the ethical principles that medicine is meant to uphold. Complex illnesses that disproportionately affect women, such as myalgic encephalomyelitis, dysautonomia, and now long COVID, are often dismissed because of stereotypes of women as hysterical and overly emotional. Black people are undertreated for pain because of persistent racist beliefs that they are less sensitive to it or have thicker skin. Disabled people often receive worse care because of ingrained beliefs that their lives are less meaningful. These biases exist-but they should be resisted. “Stigma and discrimination as a prism for allocating health-care services is already embedded in our society,” Goldberg told me. “The last thing we should do is to celebrate it.”
That is a compelling argument and provides a necessary dose of empathy for those of us who might feel betrayed by people who are unvaccinated at this point in the pandemic. Blaming individuals for these collective responsibilities and failures is of a kind with asserting that mask-wearing and vaccination are solely personal choices rather than necessary collective actions to be undertaken by communities to keep people safer. This is the same sort of individualist thinking that has people focused on their personal “carbon footprint” instead of what massive corporations, high-emissions industries, and governments should be doing to address the climate crisis.
This piece, from Ed Yong, is not at all surprising: America Is Not Ready for Omicron.
America was not prepared for COVID-19 when it arrived. It was not prepared for last winter’s surge. It was not prepared for Delta’s arrival in the summer or its current winter assault. More than 1,000 Americans are still dying of COVID every day, and more have died this year than last. Hospitalizations are rising in 42 states. The University of Nebraska Medical Center in Omaha, which entered the pandemic as arguably the best-prepared hospital in the country, recently went from 70 COVID patients to 110 in four days, leaving its staff “grasping for resolve,” the virologist John Lowe told me. And now comes Omicron.
Will the new and rapidly spreading variant overwhelm the U.S. health-care system? The question is moot because the system is already overwhelmed, in a way that is affecting all patients, COVID or otherwise. “The level of care that we’ve come to expect in our hospitals no longer exists,” Lowe said.
The real unknown is what an Omicron cross will do when it follows a Delta hook. Given what scientists have learned in the three weeks since Omicron’s discovery, “some of the absolute worst-case scenarios that were possible when we saw its genome are off the table, but so are some of the most hopeful scenarios,” Dylan Morris, an evolutionary biologist at UCLA, told me. In any case, America is not prepared for Omicron. The variant’s threat is far greater at the societal level than at the personal one, and policy makers have already cut themselves off from the tools needed to protect the populations they serve. Like the variants that preceded it, Omicron requires individuals to think and act for the collective good — which is to say, it poses a heightened version of the same challenge that the U.S. has failed for two straight years, in bipartisan fashion.
The main point:
Here, then, is the problem: People who are unlikely to be hospitalized by Omicron might still feel reasonably protected, but they can spread the virus to those who are more vulnerable, quickly enough to seriously batter an already collapsing health-care system that will then struggle to care for anyone — vaccinated, boosted, or otherwise. The collective threat is substantially greater than the individual one. And the U.S. is ill-poised to meet it.
Also from Yong: he recently cancelled his 40th birthday party because of Omicron and wrote about how he thought through the decision.
If someone got sick, I know others could too. A week later, many of my friends will spend Christmas with their own families. At best, a cluster of infections at the birthday party would derail those plans, creating days of anxious quarantine or isolation, and forcing the people I love to spend time away from their loved ones. At worst, people might unknowingly carry the virus to their respective families, which might include elderly, immunocompromised, unvaccinated, partially vaccinated, or otherwise vulnerable people. Being born eight days before Christmas creates almost the perfect conditions for one potential super-spreader event to set off many more.
As has been the case the entire pandemic, our political and public health systems are not equipped to collectively combat this virus, so it falls to individuals to make good choices for our communities. It’s a nearly impossible thing to ask to pandemic-weary folks to focus in again on making good personal choices and even harder to achieve if few are willing to do it, but goddammit we have to try.
Ed Yong: We’re Already Barreling Toward the Next Pandemic. The US is throwing too little money at high-tech, ultimately private sector solutions but much of the problem comes down to our underfunded public health system and “profoundly unequal society”.
“To be ready for the next pandemic, we need to make sure that there’s an even footing in our societal structures,” Seema Mohapatra, a health-law expert at Indiana University, told me. That vision of preparedness is closer to what 19th-century thinkers lobbied for, and what the 20th century swept aside. It means shifting the spotlight away from pathogens themselves and onto the living and working conditions that allow pathogens to flourish. It means measuring preparedness not just in terms of syringes, sequencers, and supply chains but also in terms of paid sick leave, safe public housing, eviction moratoriums, decarceration, food assistance, and universal health care. It means accompanying mandates for social distancing and the like with financial assistance for those who might lose work, or free accommodation where exposed people can quarantine from their family. It means rebuilding the health policies that Reagan began shredding in the 1980s and that later administrations further frayed. It means restoring trust in government and community through public services. “It’s very hard to achieve effective containment when the people you’re working with don’t think you care about them,” Arrianna Marie Planey, a medical geographer at the University of North Carolina at Chapel Hill, told me.
I’m just going to go ahead and say it right up front here: if you had certain expectations in May/June about how the pandemic was going to end in the US (or was even thinking it was over), you need to throw much of that mindset in the trash and start again because the Delta variant of SARS-CoV-2 has changed the game. I know this sucks to hear,1 but Delta is sufficiently different that we need to reset and stop assuming we can solely rely on the vaccines to stop Covid-19 from spreading. Ed Yong’s typically excellent piece on how delta has changed the pandemic’s endgame is helping me wrap my head around this.
But something is different now — the virus. “The models in late spring were pretty consistent that we were going to have a ‘normal’ summer,” Samuel Scarpino of the Rockefeller Foundation, who studies infectious-disease dynamics, told me. “Obviously, that’s not where we are.” In part, he says, people underestimated how transmissible Delta is, or what that would mean. The original SARS-CoV-2 virus had a basic reproduction number, or R0, of 2 to 3, meaning that each infected person spreads it to two or three people. Those are average figures: In practice, the virus spread in uneven bursts, with relatively few people infecting large clusters in super-spreading events. But the CDC estimates that Delta’s R0 lies between 5 and 9, which “is shockingly high,” Eleanor Murray, an epidemiologist at Boston University, told me. At that level, “its reliance on super-spreading events basically goes away,” Scarpino said.
In simple terms, many people who caught the original virus didn’t pass it to anyone, but most people who catch Delta create clusters of infection. That partly explains why cases have risen so explosively. It also means that the virus will almost certainly be a permanent part of our lives, even as vaccines blunt its ability to cause death and severe disease.
And a reminder, as we “argue over small measures” here in the US, that most of the world is in a much worse place:
Pandemics end. But this one is not yet over, and especially not globally. Just 16 percent of the world’s population is fully vaccinated. Many countries, where barely 1 percent of people have received a single dose, are “in for a tough year of either lockdowns or catastrophic epidemics,” Adam Kucharski, the infectious-disease modeler, told me. The U.S. and the U.K. are further along the path to endemicity, “but they’re not there yet, and that last slog is often the toughest,” he added. “I have limited sympathy for people who are arguing over small measures in rich countries when we have uncontrolled epidemics in large parts of the world.”
Where I think Yong’s piece stumbles a little is in its emphasis of the current vaccines’ protection against infection from Delta. As David Wallace-Wells explains in his piece Don’t Panic, But Breakthrough Cases May Be a Bigger Problem Than You’ve Been Told, vaccines still offer excellent protection against severe infection, hospitalization, and death, but there is evidence that breakthrough infections are more common than many public health officials are saying. The problem lies with the use of statistics from before vaccines and Delta were prevalent:
Almost all of these calculations about the share of breakthrough cases have been made using year-to-date 2021 data, which include several months before mass vaccination (when by definition vanishingly few breakthrough cases could have occurred) during which time the vast majority of the year’s total cases and deaths took place (during the winter surge). This is a corollary to the reassuring principle you might’ve heard, over the last few weeks, that as vaccination levels grow we would expect the percentage of vaccinated cases will, too — the implication being that we shouldn’t worry too much over panicked headlines about the relative share of vaccinated cases in a state or ICU but instead focus on the absolute number of those cases in making a judgment about vaccine protection across a population. This is true. But it also means that when vaccination levels were very low, there were inevitably very few breakthrough cases, too. That means that to calculate a prevalence ratio for cases or deaths using the full year’s data requires you to effectively divide a numerator of four months of data by a denominator of seven months of data. And because those first few brutal months of the year were exceptional ones that do not reflect anything like the present state of vaccination or the disease, they throw off the ratios even further. Two-thirds of 2021 cases and 80 percent of deaths came before April 1, when only 15 percent of the country was fully vaccinated, which means calculating year-to-date ratios means possibly underestimating the prevalence of breakthrough cases by a factor of three and breakthrough deaths by a factor of five. And if the ratios are calculated using data sets that end before the Delta surge, as many have been, that adds an additional distortion, since both breakthrough cases and severe illness among the vaccinated appear to be significantly more common with this variant than with previous ones.
Vaccines are still the best way to protect yourself and your community from Covid-19. The vaccines are still really good, better than we could have hoped for. But they’re not magic and with the rise of Delta (and potentially worse variants on the horizon if the virus is allowed to continue to spread unchecked and mutate), we need to keep doing the other things (masking, distancing, ventilation, etc.) in order to keep the virus in check and avoid lockdowns, school closings, outbreaks, and mass death. We’ve got the tools; we just need to summon the will and be in the right mindset.
The Atlantic’s Ed Yong is one of our great biology writers. He recently won a Pulitzer for his coverage of the COVID-19 pandemic, but it’s equally illuminating and much more fun to read him write about tapeworms or some other more benign form of life.
In this case, it’s about songbirds, which have two unusual things in common besides their love of song: they all evolved to detect and eat sugar in the form of sap and nectar [and did so in a way different from hummingbirds, who also love the sweet stuff], and they all did this in Australia, and from there spread out all over the world.
Songbirds probably evolved sweet perception about 30 million years ago, when Australia was much wetter. As the climate dried, the soils became poorer and the eucalyptus trees expanded. The forests abounded with new sources of sugar such as manna, which the songbirds were already primed to find and exploit. Perhaps the extra energy from these abundant calories allowed them to migrate over long distances and travel to other continents. Perhaps they could thrive in their new homes by finding flowers that were already baiting insects with nectar. “They are the most successful group of birds,” Eisthen told me. “You have to wonder how much of their success is due to this hidden talent, which allows them to invade new niches and feed on food sources that other animals are not exploiting.” …
Meanwhile, Sushma Reddy, an ornithologist at the University of Minnesota, points out that hummingbirds, songbirds, and parrots, three groups of birds with lots of nectar-eating species, “are also the same lineages that have convergently evolved vocal learning”—the ability to make new songs and sounds after listening to other individuals. Could these traits be related? Perhaps there’s a hidden connection between the sugary riches of Australia’s forests and the beautiful tunes that fill the air of every continent—between sweetness of palate and sweetness of voice.
Side note: Ed mentions in a parenthetical here that “fans of the board game Wingspan and its Oceania expansion will be familiar with the importance of nectar to Australian birds.” I, in fact, was not familiar with the board game Wingspan or any expansions thereof, so I looked it up:
You are bird enthusiasts—researchers, bird watchers, ornithologists, and collectors—seeking to discover and attract the best birds to your network of wildlife preserves. Each bird extends a chain of powerful combinations in one of your habitats (actions). These habitats focus on several key aspects of growth:
- Gain food tokens via custom dice in a birdfeeder dice tower
- Lay eggs using egg miniatures in a variety of colors
- Draw from hundreds of unique bird cards and play them
The winner is the player with the most points after 4 rounds.
Also, apparently it’s a card-based game, but is also available for computers via Steam. The more you know!
Ed Yong writing in The Atlantic, Individualism Is Still Sabotaging the Pandemic Response:
From its founding, the United States has cultivated a national mythos around the capacity of individuals to pull themselves up by their bootstraps, ostensibly by their own merits. This particular strain of individualism, which valorizes independence and prizes personal freedom, transcends administrations. It has also repeatedly hamstrung America’s pandemic response. It explains why the U.S. focused so intensely on preserving its hospital capacity instead of on measures that would have saved people from even needing a hospital. It explains why so many Americans refused to act for the collective good, whether by masking up or isolating themselves. And it explains why the CDC, despite being the nation’s top public-health agency, issued guidelines that focused on the freedoms that vaccinated people might enjoy. The move signaled to people with the newfound privilege of immunity that they were liberated from the pandemic’s collective problem. It also hinted to those who were still vulnerable that their challenges are now theirs alone and, worse still, that their lingering risk was somehow their fault. (“If you’re not vaccinated, that, again, is taking your responsibility for your own health into your own hands,” Walensky said.)
The pandemic demonstrated, in plain and easily understandable numbers of Covid deaths, that America is a place where the swift leave the stragglers to the wolves. I hope against hope that’ll change for the better in the future.
Because of the remarkable Covid-19 vaccines, the pandemic is easing in America. In many parts of the country, things are returning to some semblance of normal, whatever that means. But many will continue to struggle and come to terms with what happened for awhile longer. Ed Yong, What Happens When Americans Can Finally Exhale:
But there is another crucial difference between May 2020 and May 2021: People have now lived through 14 months of pandemic life. Millions have endured a year of grief, anxiety, isolation, and rolling trauma. Some will recover uneventfully, but for others, the quiet moments after adrenaline fades and normalcy resumes may be unexpectedly punishing. When they finally get a chance to exhale, their breaths may emerge as sighs. “People put their heads down and do what they have to do, but suddenly, when there’s an opening, all these feelings come up,” Laura van Dernoot Lipsky, the founder and director of the Trauma Stewardship Institute, told me. Lipsky has spent decades helping people navigate the consequences of natural disasters, mass shootings, and other crises. “As hard as the initial trauma is,” she said, “it’s the aftermath that destroys people.”
And it wasn’t just the pandemic:
Not everyone will feel this way. Perhaps most Americans won’t. In past work, Silver, the UC Irvine psychologist, found that even communities that go through extreme traumas, such as years of daily rocket fire, can show low levels of PTSD. Three factors seem to protect them: confidence in authorities, a sense of belonging, and community solidarity. In the U.S., the pandemic eroded all three. It reduced trust in institutions, separated people from their loved ones, and widened political divisions. It was something of a self-reinforcing disaster, exacerbating the conditions that make recovery harder.
Also, let’s not forget: “Globally, the pandemic is set to kill more people in 2021 than in 2020.”
In the Atlantic, Ed Yong checks back in with the long-haulers, people who are still experiencing Covid-19 symptoms months after their initial infection. (Read his previous article from early June.)
Lauren Nichols has been sick with COVID-19 since March 10, shortly before Tom Hanks announced his diagnosis and the NBA temporarily canceled its season. She has lived through one month of hand tremors, three of fever, and four of night sweats. When we spoke on day 150, she was on her fifth month of gastrointestinal problems and severe morning nausea. She still has extreme fatigue, bulging veins, excessive bruising, an erratic heartbeat, short-term memory loss, gynecological problems, sensitivity to light and sounds, and brain fog. Even writing an email can be hard, she told me, “because the words I think I’m writing are not the words coming out.” She wakes up gasping for air twice a month. It still hurts to inhale.
As Yong says in a thread about the article: “The pandemic is going to create a large wave of chronically disabled people.” Once again for the people in the back: this is not just the flu. The flu does not incapacitate otherwise healthy people like this. I know at least two long-haulers personally and am astounded on a daily basis by how casually some Americans continue to regard Covid-19.
More than 90 percent of long-haulers whom Putrino has worked with also have “post-exertional malaise,” in which even mild bouts of physical or mental exertion can trigger a severe physiological crash. “We’re talking about walking up a flight of stairs and being out of commission for two days,” Putrino said. This is the defining symptom of myalgic encephalomyelitis, or chronic fatigue syndrome. For decades, people with ME/CFS have endured the same gendered gaslighting that long-haulers are now experiencing. They’re painfully familiar with both medical neglect and a perplexing portfolio of symptoms.
You can read Seabiscuit author Laura Hillenbrand’s excellent article on her chronic fatigue syndrome diagnosis and how difficult it is for people with chronic conditions like this to get the right diagnosis and to get family and friends to believe what’s going on.
Also, Yong should win all the awards this year for his pandemic coverage. It has been simply outstanding.
The Atlantic’s Ed Yong interviewed several people who, like thousands of others around the world, have been experiencing symptoms of Covid-19 for months now, indicating that the disease is chronic for some. Thousands Who Got COVID-19 in March Are Still Sick:
I interviewed nine of them for this story, all of whom share commonalities. Most have never been admitted to an ICU or gone on a ventilator, so their cases technically count as “mild.” But their lives have nonetheless been flattened by relentless and rolling waves of symptoms that make it hard to concentrate, exercise, or perform simple physical tasks. Most are young. Most were previously fit and healthy. “It is mild relative to dying in a hospital, but this virus has ruined my life,” LeClerc said. “Even reading a book is challenging and exhausting. What small joys other people are experiencing in lockdown-yoga, bread baking-are beyond the realms of possibility for me.”
One of those who has been sick for months is Paul Garner, a professor of infectious diseases:
It “has been like nothing else on Earth,” said Paul Garner, who has previously endured dengue fever and malaria, and is currently on day 77 of COVID-19. Garner, an infectious-diseases professor at the Liverpool School of Tropical Medicine, leads a renowned organization that reviews scientific evidence on preventing and treating infections. He tested negative on day 63. He had waited to get a COVID-19 test partly to preserve them for health-care workers, and partly because, at one point, he thought he was going to die. “I knew I had the disease; it couldn’t have been anything else,” he told me. I asked him why he thought his symptoms had persisted. “I honestly don’t know,” he said. “I don’t understand what’s happening in my body.”
Garner wrote about his experience for BMJ.
The illness went on and on. The symptoms changed, it was like an advent calendar, every day there was a surprise, something new. A muggy head; acutely painful calf; upset stomach; tinnitus; pins and needles; aching all over; breathlessness; dizziness; arthritis in my hands; weird sensation in the skin with synthetic materials. Gentle exercise or walking made me worse — I would feel absolutely dreadful the next day. I started talking to others. I found a marathon runner who had tried 8 km in her second week, which caused her to collapse with rigors and sleep for 24 hours. I spoke to others experiencing weird symptoms, which were often discounted by those around them as anxiety, making them doubt themselves.
We still have no idea what the long-term effects of this disease are going to be. But it is definitely not the flu. And I remain unwilling to risk myself or my family getting it.
As Ed Yong notes in his helpful overview of the pandemic, this is such a huge and quickly moving event that it’s difficult to know what’s happening. Lately, I’ve been seeking information on Covid-19’s presenting symptoms after seeing a bunch of anecdotal data from various sources.
In the early days of the epidemic (January, February, and into March), people were told by the CDC and other public health officials to watch out for three specific symptoms: fever, a dry cough, and shortness of breath. In many areas, testing was restricted to people who exhibited only those symptoms. Slowly, as more data is gathered, the profile of the presenting symptoms has started to shift. From a New York magazine piece by David Wallace-Wells on Monday:
While the CDC does list fever as the top symptom of COVID-19, so confidently that for weeks patients were turned away from testing sites if they didn’t have an elevated temperature, according to the Journal of the American Medical Association, as many as 70 percent of patients sick enough to be admitted to New York State’s largest hospital system did not have a fever.
Over the past few months, Boston’s Brigham and Women’s Hospital has been compiling and revising, in real time, treatment guidelines for COVID-19 which have become a trusted clearinghouse of best-practices information for doctors throughout the country. According to those guidelines, as few as 44 percent of coronavirus patients presented with a fever (though, in their meta-analysis, the uncertainty is quite high, with a range of 44 to 94 percent). Cough is more common, according to Brigham and Women’s, with between 68 percent and 83 percent of patients presenting with some cough — though that means as many as three in ten sick enough to be hospitalized won’t be coughing. As for shortness of breath, the Brigham and Women’s estimate runs as low as 11 percent. The high end is only 40 percent, which would still mean that more patients hospitalized for COVID-19 do not have shortness of breath than do. At the low end of that range, shortness of breath would be roughly as common among COVID-19 patients as confusion (9 percent), headache (8 to 14 percent), and nausea and diarrhea (3 to 17 percent).
Recently, as noted by the Washington Post, the CDC has changed their list of Covid-19 symptoms to watch out for. They now list two main symptoms (cough & shortness of breath) and several additional symptoms (fever, chills, repeated shaking with chills, muscle pain, headache, sore throat, new loss of taste or smell). They also note that “this list is not all inclusive”. Compare that with their list from mid-February.
In addition, there’s evidence that children might have different symptoms (including stomach issues or diarrhea), doctors are reporting seeing “COVID toes” on some patients, and you might want to look at earlier data from these three studies about symptoms observed in Wuhan and greater China.
The reason I’m interested in this shift in presenting symptoms is that on the last day or two of my trip to Asia, I got sick — and I’ve been wondering if it was Covid-19.
Here’s the timeline: starting on Jan 21, I was in Saigon, Vietnam for two weeks, then in Singapore for 4 days, and then Doha, Qatar for 48 hours. The day I landed in Doha, Feb 9, I started to feel a little off, and definitely felt sick the next day. I had a sore throat, headache, and congestion (stuffy nose) for the first few days. There was also some fatigue/tiredness but I was jetlagged too so… All the symptoms were mild and it felt like a normal cold to me. Here’s how I wrote about it in my travelogue:
I got sick on the last day of the trip, which turned into a full-blown cold when I got home. I dutifully wore my mask on the plane and in telling friends & family about how I was feeling, I felt obliged to text “***NOT*** coronavirus, completely different symptoms!!”
I flew back to the US on Feb 11 (I wore a mask the entire time in the Doha airport, on the plane, and even in the Boston airport, which no one else was doing). I lost my sense of taste and smell for about 2 days, which was a little unnerving but has happened to me with past colds. At no point did I have even the tiniest bit of fever or shortness of breath. The illness did drag on though — I felt run-down for a few weeks and a very slight cough that developed about a week and a half after I got sick lingered for weeks.
According to guidance from the WHO, CDC, and public health officials at the time, none of my initial symptoms were a match for Covid-19. I thought about getting a test or going to the doctor, but in the US in mid-February, and especially in Vermont, there were no tests available for someone with a mild cold and no fever. But looking at the CDC’s current list of symptoms — which include headache, sore throat, and new loss of taste or smell — and considering that I’d been in Vietnam and Singapore when cases were reported in both places, it seems plausible to me that my illness could have been a mild case of Covid-19. Hopefully it wasn’t, but I’ll be getting an antibody test once they are (hopefully) more widely available, even though the results won’t be super reliable.
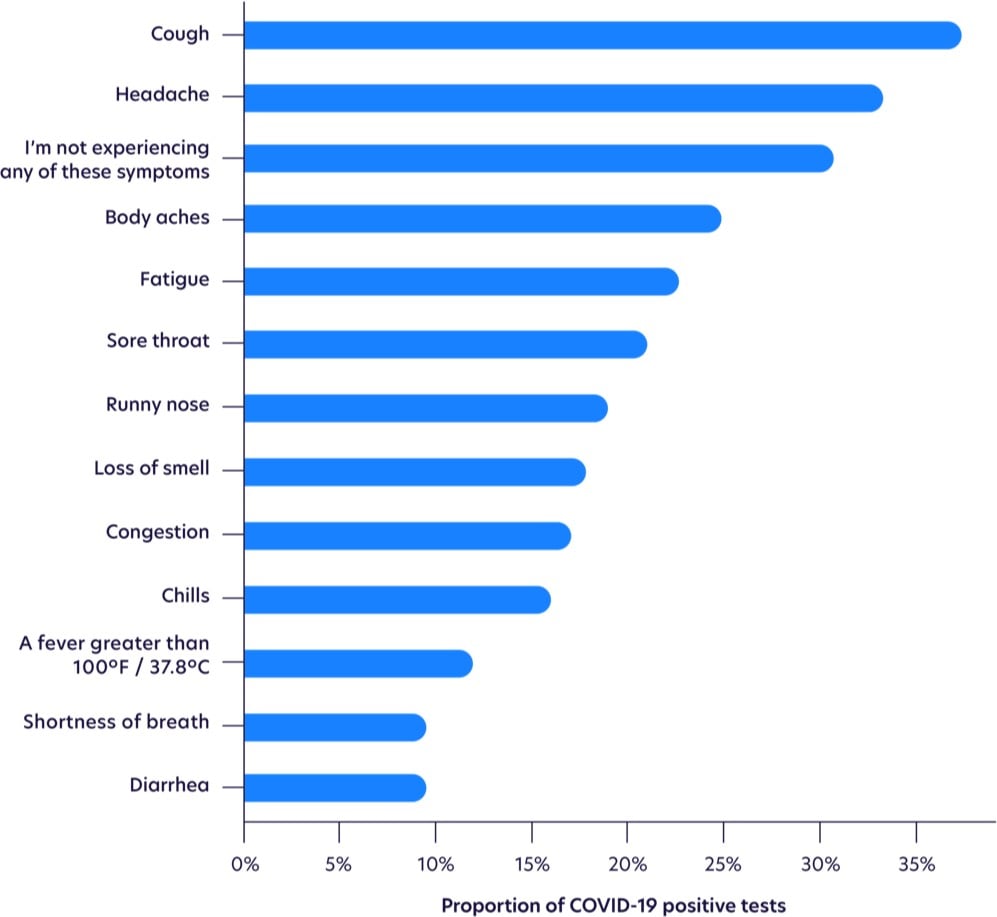
Update: More on the changing profile of Covid-19 symptoms from a sample size of more than 30,000 tests.
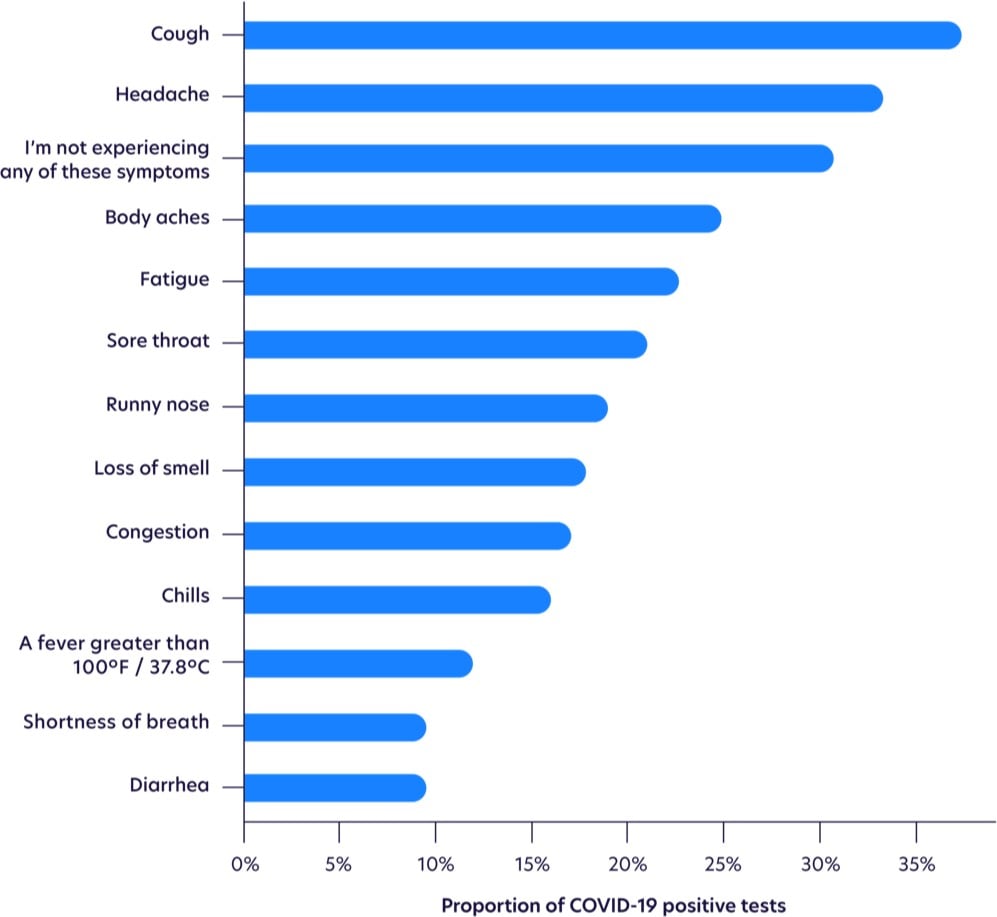
Fever is waaay down on the list.
While not as common as other symptoms, loss of smell was the most highly correlated with testing positive, as shown with odds ratios below, after adjusting for age and gender. Those with loss of smell were more likely to test positive for COVID-19 than those with a high fever.
Seeing this makes me think more than ever that I had it. I had three of the top five symptoms, plus an eventual cough (the most common symptom) and a loss of smell & taste (the most highly correlated symptom). The timing of the onset of my symptoms (my first day in Qatar) indicates that I probably got infected on my last day in Vietnam, in transit from Vietnam to Singapore (1 2-hr plane ride, 2 airports, 1 taxi, 1 train ride), or on my first day in Singapore. But I went to so many busy places during that time that it’s impossible to know where I might have gotten infected (or who I then went on to unwittingly infect).
Update: A few weeks ago, I noticed some horizontal lines on several of my toenails, a phenomenon I’d never seen before. When I finally googled it, I discovered they’re called Beau’s lines and they can show up when the body has been stressed by illness or disease. Hmm. From the Wikipedia page:
Some other reasons for these lines include trauma, coronary occlusion, hypocalcaemia, and skin disease. They may be a sign of systemic disease, or may also be caused by an illness of the body, as well as drugs used in chemotherapy, or malnutrition. Beau’s lines can also be seen one to two months after the onset of fever in children with Kawasaki disease.
From the Mayo Clinic:
Conditions associated with Beau’s lines include uncontrolled diabetes and peripheral vascular disease, as well as illnesses associated with a high fever, such as scarlet fever, measles, mumps and pneumonia.
From the estimated growth of my nails, it seems as though whatever disruption that caused the Beau’s lines happened 5-6 months ago, which lines up with my early February illness that I believe was Covid-19. Covid-19 can definitely affect the vascular systems of infected persons. Kawasaki disease is a vascular disease and a similar syndrome in children resulting from SARS-CoV-2 exposure is currently under investigation. And here’s a paper from December 1971 that tracked the development of Beau’s lines in several people who were ill during the 1968 flu pandemic (an H3N2 strain of the influenza A virus) — coronaviruses and influenza viruses are different but this is still an indicator that viruses can result in Beau’s lines. “Covid toe” has been observed in many Covid-19 patients. Harvard dermatologist and epidemiologist Dr. Esther Freeman reports that people may be experiencing hair loss due to Covid-19.
I couldn’t find any scientific literature about the possible correlation of Covid-19 and Beau’s lines, but I did find some suggestive anecdotal information. I found several people on Twitter who noticed lines in their nails (both fingers and toes) and who also have confirmed or suspected cases of Covid-19. And if you go to Google’s search bar and type “Beau’s lines c”, 3 of the 10 autocomplete suggestions are related to Covid-19, which indicates that people are searching for it (but not enough to register on Google Trends).
But I am definitely intrigued. Are dermatologists and podiatrists seeing Beau’s lines on patients who have previously tested positive for Covid-19? Have people who have tested positive noticed them? Email me at [email protected] if you have any info about this; I’d love to get to the bottom of this.
The Atlantic’s Ed Yong has written his second long article about the Covid-19 pandemic about what happens next and what a roadmap to dealing with the next phase of the crisis might look like.
As I wrote last month, the only viable endgame is to play whack-a-mole with the coronavirus, suppressing it until a vaccine can be produced. With luck, that will take 18 to 24 months. During that time, new outbreaks will probably arise. Much about that period is unclear, but the dozens of experts whom I have interviewed agree that life as most people knew it cannot fully return. “I think people haven’t understood that this isn’t about the next couple of weeks,” said Michael Osterholm, an infectious-disease epidemiologist at the University of Minnesota. “This is about the next two years.”
The pandemic is not a hurricane or a wildfire. It is not comparable to Pearl Harbor or 9/11. Such disasters are confined in time and space. The SARS-CoV-2 virus will linger through the year and across the world. “Everyone wants to know when this will end,” said Devi Sridhar, a public-health expert at the University of Edinburgh. “That’s not the right question. The right question is: How do we continue?”

Have you been wearing a face mask when going out in public recently? There’s been a lot of debate recently about whether they are effective in keeping people safe from COVID-19 infection, and it’s been really challenging to find good information. After reading several things over the past few days, I have concluded that wearing a mask in public is a helpful step I can take to help keep myself and others safe, with the important caveat that healthcare workers need access to masks before the rest of us (see below). In particular, I found this extensive review of the medical and scientific literature on mask & respirator use helpful, including why research on mask efficacy is so hard to do and speculation on why the CDC and WHO generally don’t recommend wearing them.
I was able to find one study like this outside of the health care setting. Some people with swine flu travelled on a plane from New York to China, and many fellow passengers got infected. Some researchers looked at whether passengers who wore masks throughout the flight stayed healthier. The answer was very much yes. They were able to track down 9 people who got sick on the flight and 32 who didn’t. 0% of the sick passengers wore masks, compared to 47% of the healthy passengers. Another way to look at that is that 0% of mask-wearers got sick, but 35% of non-wearers did. This was a significant difference, and of obvious applicability to the current question.
See also this review of relevant scientific literature, this NY Times piece, this Washington Post opinion piece by Jeremy Howard (who is on a Twitter mission to get everyone to wear masks):
When historians tally up the many missteps policymakers have made in response to the coronavirus pandemic, the senseless and unscientific push for the general public to avoid wearing masks should be near the top.
The evidence not only fails to support the push, it also contradicts it. It can take a while for official recommendations to catch up with scientific thinking. In this case, such delays might be deadly and economically disastrous. It’s time to make masks a key part of our fight to contain, then defeat, this pandemic. Masks effective at “flattening the curve” can be made at home with nothing more than a T-shirt and a pair of scissors. We should all wear masks — store-bought or homemade — whenever we’re out in public.
At the height of the HIV crisis, authorities did not tell people to put away condoms. As fatalities from car crashes mounted, no one recommended avoiding seat belts. Yet in a global respiratory pandemic, people who should know better are discouraging Americans from using respiratory protection.
I have to admit that I have not been wearing a mask out in public — I’ve been to the grocery store only three times in the past two weeks, I go at off-hours, and it’s rural Vermont, so there’s not actually that many people about (e.g. compared to Manhattan). But I’m going to start wearing one in crowded places (like the grocery store) because doing so could a) safeguard others against my possible infection (because asymptomatic people can still be contagious), b) make it less likely for me to get infected, and c) provide a visible signal to others in my community to normalize mask wearing. As we’ve seen in epidemic simulations, relatively small measures can have outsize effects in limiting later infections & deaths, and face masks, even if a tiny bit effective, can have a real impact.
Crucially, the available research and mask advocates stress the importance of wearing masks properly and responsibly. Here are some guidelines I compiled about responsible mask usage:
Don’t buy masks (or use new masks you might have at home) while there is a shortage for healthcare workers, especially not N95 respirators (which are difficult to use properly anyway). Make a mask at home. Skiers & snowboarders, wear your buffs or ski masks. Donate any unused masks or respirators you may have to healthcare workers.
Make sure your mask fits properly — limit any gaps between the mask and your face as much as you can. (Facial hair can limit mask effectiveness.)
While wearing your mask in public, don’t fuss with it — touching your face is bad, remember? Wear it at home for a few hours to get used to the sensation. Then when you’re ready to go out, put it on properly and don’t touch it again until you’re back home (or in the car or whatever). Part of the point of the mask is for you to touch your face less.
Limit reuse of potentially contaminated masks. Discard or, if possible, wash or disinfect masks after public usage or at the end of the day.
Wearing a mask doesn’t mean you can safely go do a bunch of things without fear of getting infected. The idea here is to protect yourself while engaging in necessary activities in public. Wearing a mask doesn’t mean you can visit grandma safely or discard the six-feet-away rule.
Don’t do anything stupid like spraying your mask with a household cleaner that contains bleach and put it on. Come on.
So that’s what I’ve personally concluded from all my reading. I hope wearing masks can help keep us a little safer during all of this.
Update: From Ferris Jabr at Wired, It’s Time to Face Facts, America: Masks Work.
It is unequivocally true that masks must be prioritized for health care workers in any country suffering from a shortage of personal protective equipment. But the conflicting claims and guidelines regarding their use raise three questions of the utmost urgency: Do masks work? Should everyone wear them? And if there aren’t enough medical-grade masks for the general public, is it possible to make a viable substitute at home? Decades of scientific research, lessons from past pandemics, and common sense suggest the answer to all of these questions is yes.
Update: The Atlantic’s Ed Yong weighs in on masks:
In Asia, masks aren’t just shields. They’re also symbols. They’re an affirmation of civic-mindedness and conscientiousness, and such symbols might be important in other parts of the world too. If widely used, masks could signal that society is taking the pandemic threat seriously. They might reduce the stigma foisted on sick people, who would no longer feel ashamed or singled out for wearing one. They could offer reassurance to people who don’t have the privilege of isolating themselves at home, and must continue to work in public spaces. “My staff have also mentioned that having a mask reminds them not to touch their face or put a pen in their mouth,” Bourouiba noted.
He also writes about something I’ve been wondering about: is the virus airborne, what does that even mean, when will we know for sure, and how should that affect our behavior in the meantime?
These particles might not even have been infectious. “I think we’ll find that like many other viruses, [SARS-CoV-2] isn’t especially stable under outdoor conditions like sunlight or warm temperatures,” Santarpia said. “Don’t congregate in groups outside, but going for a walk, or sitting on your porch on a sunny day, are still great ideas.”
You could tie yourself in knots gaming out the various scenarios that might pose a risk outdoors, but Marr recommends a simple technique. “When I go out now, I imagine that everyone is smoking, and I pick my path to get the least exposure to that smoke,” she told me. If that’s the case, I asked her, is it irrational to hold your breath when another person walks past you and you don’t have enough space to move away? “It’s not irrational; I do that myself,” she said. “I don’t know if it makes a difference, but in theory it could. It’s like when you walk through a cigarette plume.”
And from the WHO, here’s a video on how to wear a mask properly.
Update: One of the reasons I started to wear a mask when I go out in public was to “provide a visible signal to others in my community to normalize mask wearing”. Maciej Cegłowski’s post touches on this and other reasons to wear a mask that don’t directly have to do with avoiding infection.
A mask is a visible public signal to strangers that you are trying to protect their health. No other intervention does this. It would be great if we had a soap that turned our hands gold for an hour, so everyone could admire our superb hand-washing technique. But all of the behaviors that benefit public health are invisible, with the exception of mask wearing.
If I see you with a mask on, it shows me you care about my health, and vice versa. This dramatically changes what it feels like to be in a public space. Other people no longer feel like an anonymous threat; they are now your teammates in a common struggle.
From Ed Yong at the Atlantic, a great article on the current state of the pandemic in the United States, what will happen over the next few months, how it will end, and what the aftermath will be.
With little room to surge during a crisis, America’s health-care system operates on the assumption that unaffected states can help beleaguered ones in an emergency. That ethic works for localized disasters such as hurricanes or wildfires, but not for a pandemic that is now in all 50 states. Cooperation has given way to competition; some worried hospitals have bought out large quantities of supplies, in the way that panicked consumers have bought out toilet paper.
Partly, that’s because the White House is a ghost town of scientific expertise. A pandemic-preparedness office that was part of the National Security Council was dissolved in 2018. On January 28, Luciana Borio, who was part of that team, urged the government to “act now to prevent an American epidemic,” and specifically to work with the private sector to develop fast, easy diagnostic tests. But with the office shuttered, those warnings were published in The Wall Street Journal, rather than spoken into the president’s ear. Instead of springing into action, America sat idle.
Rudderless, blindsided, lethargic, and uncoordinated, America has mishandled the COVID-19 crisis to a substantially worse degree than what every health expert I’ve spoken with had feared. “Much worse,” said Ron Klain, who coordinated the U.S. response to the West African Ebola outbreak in 2014. “Beyond any expectations we had,” said Lauren Sauer, who works on disaster preparedness at Johns Hopkins Medicine. “As an American, I’m horrified,” said Seth Berkley, who heads Gavi, the Vaccine Alliance. “The U.S. may end up with the worst outbreak in the industrialized world.”
If you’ve been reading obsessively about the pandemic, there’s not a lot new in here, but Yong lays the whole situation out very clearly and succinctly (he easily could have gone twice as long). The section on potential after effects was especially interesting:
Pandemics can also catalyze social change. People, businesses, and institutions have been remarkably quick to adopt or call for practices that they might once have dragged their heels on, including working from home, conference-calling to accommodate people with disabilities, proper sick leave, and flexible child-care arrangements. “This is the first time in my lifetime that I’ve heard someone say, ‘Oh, if you’re sick, stay home,’” says Adia Benton, an anthropologist at Northwestern University. Perhaps the nation will learn that preparedness isn’t just about masks, vaccines, and tests, but also about fair labor policies and a stable and equal health-care system. Perhaps it will appreciate that health-care workers and public-health specialists compose America’s social immune system, and that this system has been suppressed.
Aspects of America’s identity may need rethinking after COVID-19. Many of the country’s values have seemed to work against it during the pandemic. Its individualism, exceptionalism, and tendency to equate doing whatever you want with an act of resistance meant that when it came time to save lives and stay indoors, some people flocked to bars and clubs. Having internalized years of anti-terrorism messaging following 9/11, Americans resolved to not live in fear. But SARS-CoV-2 has no interest in their terror, only their cells.
I really hope that Betteridge’s law is wrong about that headline I wrote.
Science writer Ed Yong noticed that the stories he was writing quoted sources that were disproportionately male. Using a spreadsheet to track who he contacted for stories and a few extra minutes per piece, Yong set about changing that gender imbalance.
Skeptics might argue that I needn’t bother, as my work was just reflecting the present state of science. But I don’t buy that journalism should act simply as society’s mirror. Yes, it tells us about the world as it is, but it also pushes us toward a world that could be. It is about speaking truth to power, giving voice to the voiceless. And it is a profession that actively benefits from seeking out fresh perspectives and voices, instead of simply asking the same small cadre of well-trod names for their opinions.
Another popular critique is that I should simply focus on finding the most qualified people for any given story, regardless of gender. This point seems superficially sound, but falls apart at the gentlest scrutiny. How exactly does one judge “most qualified”? Am I to list all the scientists in a given field and arrange them by number of publications, awards, or h-index, and then work my way down the list in descending order? Am I to assume that these metrics somehow exist in a social vacuum and are not themselves also influenced by the very gender biases that I am trying to resist? It would be crushingly naïve to do so.
Journalism and science both work better with the inclusion and participation of a diverse set of voices bent on the pursuit of truth.
Update: NY Times’ columnist David Leonhardt conducted his own experiment and discovered I’m Not Quoting Enough Women.
Blue Planet II, the latest BBC nature documentary narrated by David Attenborough, is finally set to air in the US this Saturday on BBC America, AMC, and other networks. Here’s a five-minute preview…if this doesn’t pique your interest, you might actually be dead:
In a review of the program at The Atlantic, Ed Yong makes a bold declaration:
Blue Planet II is the greatest nature series that the BBC has ever produced.
Coming on the heels of Planet Earth II, which I thought was the best thing I watched last year, that’s really saying something. Here’s Yong on the difference between the two:
Who can forget the marine iguanas of Planet Earth II, escaping from the jaws of hungry racer snakes? But in chasing drama, some of the shows became thinner and messier. Many episodes of Planet Earth II felt like glorious visual listicles — selections of (admittedly awesome) set pieces woven together by the flimsiest of narrative gossamer.
By contrast, the threads that hold Blue Planet II together are thick and tightly woven. Each episode flows. For example, the second episode, on the deep ocean, achieves narrative depth through actual depth, sinking deeper and deeper so that each new spectacle is anchored in space. Where previous series felt like they sacrificed the storytelling craft and educational density for technical wizardry and emotional punch, Blue Planet II finally marries all of that together.
Blue Planet II was watched by more people in the UK than Planet Earth II and has seemingly influenced the UK government’s stance on pollution:
Cutting plastic pollution is the focus of a series of proposals being considered by the UK environment secretary, Michael Gove, who has said he was “haunted” by images of the damage done to the world’s oceans shown in David Attenborough’s Blue Planet II TV series.
The government is due to announce a 25-year plan to improve the UK’s environmental record in the new year. Gove is understood to be planning to introduce refundable deposits on plastic drinks bottles, alongside other measures.
I got a sneak peek at the first few episodes of Blue Planet II, and it certainly is a great program. I watched it with my kids and they were riveted the entire time. After the fourth or fifth episode, my son said, “I think I like this better than Planet Earth II.” I’m not quite sure it’s peak Attenborough — I’m still partial to Planet Earth II — but it’s still a must-see and I’m certainly not going to argue with Ed Yong and my son about it.
Researchers at Harvard have come up with a novel way of studying how bacteria evolve to become drug resistant. They set up a large petri dish about the same shape as a football field with no antibiotics in the end zones and increasingly higher doses of antibiotics toward the center. They placed some bacteria in both end zones and filmed the results as the bacteria worked its way toward the center of the field, evolving drug resistance as it went. Ed Yong explains:
What you’re seeing in the movie is a vivid depiction of a very real problem. Disease-causing bacteria and other microbes are increasingly evolving to resist our drugs; by 2050, these impervious infections could potentially kill ten million people a year. The problem of drug-resistant infections is terrifying but also abstract; by their nature, microbes are invisible to the naked eye, and the process by which they defy our drugs is even harder to visualise.
But now you can: just watch that video again. You’re seeing evolution in action. You’re watching living things facing down new challenges, dying, competing, thriving, invading, and adapting — all in a two-minute movie.
Watch the video…it’s wild. What’s most interesting — or scary as hell — is that once the drug resistance gets going, it builds up a pretty good momentum. There’s a pause at the first boundary as the evolutionary process blindly hammers away at the problem, but after the bacteria “learn” drug resistance, the further barriers are breached much more quickly, even before the previous zones are fully populated.
Antonie van Leeuwenhoek ran a draper’s shop and was a local politician in Delft, Netherlands in the mid-17th century. During this time, he developed an interest in making lenses and hit upon a technique for making lenses with extremely high magnifications for the time, 270x and perhaps even 500x normal magnification. These lenses allowed him to discover that there were tiny organisms living in his mouth.
Ed Yong, Joss Fong, and Julia Belluz discuss van Leeuwenhoek’s achievement and microorganisms in general in the video above and in an interview.
It is undeniable that antibiotics have been a tremendous health good, maybe one of the greatest health goods of all time. They have brought so many infectious diseases to heel and saved so many lives.
But it’s also clear that they have negative effects on our microbiome. So they are indiscriminate weapons. They kill the microbes that we depend upon and that are good for us as well as the ones that are causing disease and causing us harm. They’re like nukes, rather than precision weapons.
So we’re in a difficult situation now, where on the one hand we’re running out of antibiotics, and the rise of antibiotic-resistant bacteria is a huge public health threat. But at the same time we’re aware of the need to preserve the microbiome.
Yong just came out with a book on microbes called I Contain Multitudes. (Perhaps Whitman was speaking literally?)
Crackerjack science writer Ed Yong is coming out with his very first book in a month’s time. It’s called I Contain Multitudes (good title!) and is about “astonishing partnerships between animals and microbes”.
Every animal, whether human, squid, or wasp, is home to millions of bacteria and other microbes. Ed Yong, whose humor is as evident as his erudition, prompts us to look at ourselves and our animal companions in a new light-less as individuals and more as the interconnected, interdependent multitudes we assuredly are.
The microbes in our bodies are part of our immune systems and protect us from disease. In the deep oceans, mysterious creatures without mouths or guts depend on microbes for all their energy. Bacteria provide squid with invisibility cloaks, help beetles to bring down forests, and allow worms to cause diseases that afflict millions of people.
I will read anything described as “like a David Attenborough series shot through a really good microscope”.
Update: Bill Gates liked I Contain Multitudes so much he sat down for a chat with Yong to discuss the particulars.
We are also utterly inseparable from them. Yong illustrates that we are at least as much microbe as human. We literally have more microbial cells living inside our bodies than human cells. And even the cells we label “human” are part microbe. With the exception of red blood cells and sperm, all our cells are powered by mitochondria, which are likely the descendants of ancient bacteria that became integrated into the type of cells that subsequently gave rise to all complex life.
Scientists have discovered the first promising new antibiotic in 25 years. And even better, says Ed Yong, is that the antibiotic in question is “resistant to resistance”.
A team of scientists led by Kim Lewis from Northeastern University have identified a new antibiotic called teixobactin, which kills some kinds of bacteria by preventing them from building their outer coats. They used it to successfully treat antibiotic-resistant infections in mice. And more importantly, when they tried to deliberately evolve strains of bacteria that resist the drug, they failed. Teixobactin appears resistant to resistance.
Bacteria will eventually develop ways of beating teixobactin — remember Orgel — but the team are optimistic that it will take decades rather than years for this to happen. That buys us time.
…and also that the process by which teixobactin was discovered is the real breakthrough:
Teixobactin isn’t even the most promising part of its own story. That honour falls on the iChip-the tool that the team used to discover the compound. Teixobactin is a fish; the iChip is the rod. Having the rod guarantees that we’ll get more fish-and we desperately need more.




Socials & More