A Framework for the Equitable Allocation of a COVID-19 Vaccine
Now that the preliminary results of various Covid-19 vaccine trials are coming out (and looking promising), attention is turning to the eventual distribution of the vaccines. The logistics of getting the doses out to hospitals, clinics, and doctor’s offices is one concern but so is the question of who should get vaccinated first. Supplies of the vaccines will be limited at first, so we’ll need to decide as a society what distribution method is most fair and is of the most benefit to the greatest number of people.
To this end, and in response to a request by the CDC and NIH, the National Academies of Sciences, Engineering, and Medicine formed a committee to produce a report called Framework for Equitable Allocation of COVID-19 Vaccine. The 252-page report is available to the public for free to read online or download.
In addition several recommendations — including that the vaccine be distributed to everyone free of charge — a central feature of the report is a four-phase system of vaccine distribution, summarized in this graphic:
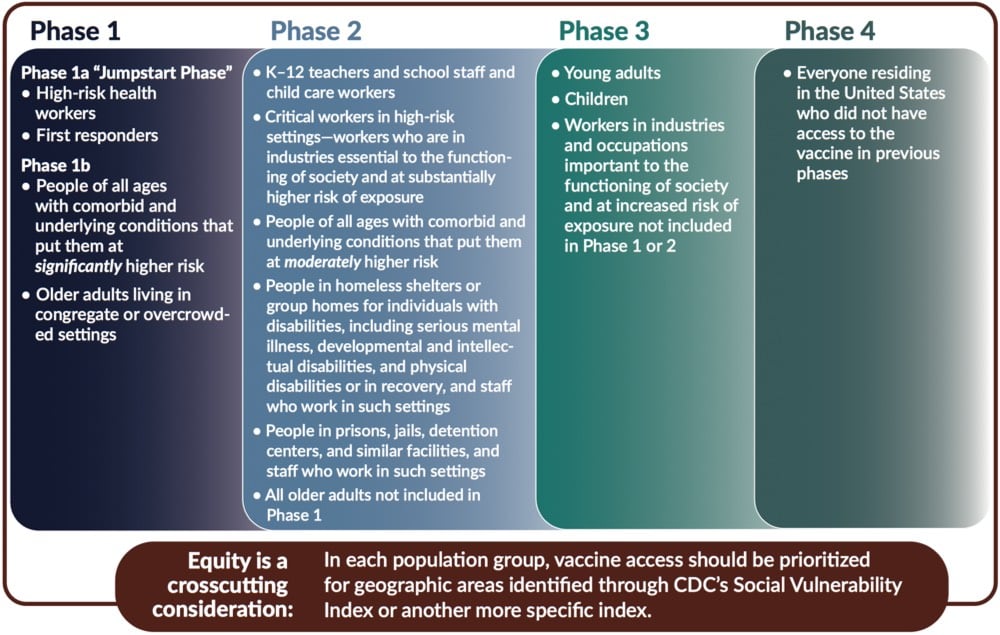
I’d like to stress that this graphic does not show all groups of people included in each phase — please consult the text of the report for that before you go sharing that graphic on social media without context. For example, here’s the full description for “high-risk health workers” in Phase 1a:
This group includes frontline health care workers (who are in hospitals, nursing homes, or providing home care) who either (1) work in situations where the risk of SARS-CoV-2 transmission is higher, or (2) are at an elevated risk of transmitting the infection to patients at higher risk of mortality and severe morbidity. These individuals — who are themselves unable to avoid exposure to the virus — play a critical role in ensuring that the health system can care for COVID-19 patients.
These groups include not only clinicians (e.g., nurses, physicians, respiratory technicians, dentists and hygienists) but also other workers in health care settings who meet the Phase 1a risk criteria (e.g., nursing assistants, environmental services staff, assisted living facility staff, long-term care facility staff, group home staff, and home caregivers). The health care settings employing these workers who are at increased risk of exposure to the virus may also include ambulatory and urgent care clinics; dialysis centers; blood, organ, and tissue donation facilities; and other non-hospital health care facilities. Finally, there are community and family settings where care for infected patients occurs. Not all the workers in these settings are paid for their labor, but, while they are caring for infected people, they all need to be protected from the virus.
Situations associated with higher risk of transmission include caring for COVID-19 patients, cleaning areas where COVID-19 patients are admitted, treated, and housed, and performing procedures with higher risk of aerosolization such as endotracheal intubation, bronchoscopy, suctioning, turning the patient to the prone position, disconnecting the patient from the ventilator, invasive dental procedures and exams, invasive specimen collection, and cardiopulmonary resuscitation. In addition, there are other frontline health care workers who, if they have uncontrolled exposure to the patients or the public in the course of their work, should be in this initial phase. This group includes those individuals distributing or administering the vaccine — especially in areas of higher community transmission — such as pharmacists, plasma and blood donation workers, public health nurses, and other public health and emergency preparedness workers. The committee also includes morticians, funeral home workers, and other death care professionals involved in handling bodies as part of this high-risk group.
The report declines to list specific industries which would be covered in Phase 2’s “critical workers in high-risk settings” but generally says:
The industries in which these critical workers are employed are essential to keeping society and the economy functioning. Since the beginning of the pandemic, millions of people have been going to work and risking exposure to the virus to ensure that markets have food; drug stores have pharmaceutical products; public safety and order are maintained; mail and packages are delivered; and buses, trains, and planes are operating.
Note also the text at the bottom of the graphic: they recommend that within each phase, priority be given to geographic areas where folks are more socially vulnerable in situations like these (e.g. as represented in the CDC’s Social Vulnerability Index).
In developing this phased approach, the committee focused on those who are at the most risk of exposure, severe illness or death, and passing along the virus to others as well as critical workers:
Risk of acquiring infection: Individuals have higher priority to the extent that they have a greater probability of being in settings where SARS-CoV-2 is circulating and of being exposed to a sufficient dose of the virus.
Risk of severe morbidity and mortality: Individuals have higher priority to the extent that they have a greater probability of severe disease or death if they acquire infection.
Risk of negative societal impact: Individuals have higher priority to the extent that societal function and other individuals’ lives and livelihood depend on them directly and would be imperiled if they fell ill.
Risk of transmitting infection to others: Individuals have higher priority to the extent that there is a higher probability of their transmitting the infection to others.
You should read (or at least skim) the full report for more information about the plan and the rationale behind it.
On a personal parting note, as someone who is squarely in the 5-15% of Americans covered in Phase 4 — more specifically: as a 40-something straight white man who non-essentially works from home, isn’t low-income, doesn’t socialize widely even under normal circumstances, and should probably be the very last person on this whole Earth scheduled to be vaccinated under an equitable framework — I am content to wait my turn should the US adopt this framework or something like it.1 Distributing vaccines to those who need them most is absolutely the right thing to do, both ethically and from the standpoint of getting society “back to normal” as quickly as possible and with as little additional death and suffering as possible.
Being that equity often isn’t America’s thing, especially during the pandemic, I could see this going either way. And even if this framework is adopted, those who can afford it will undoubtably be able to procure themselves a dose right alongside those medical workers in Phase 1a.↩


Stay Connected