SARS-CoV-2, An Emerging Portrait
From Nature’s David Cyranoski, a piece that takes a look at what the latest research says about SARS-CoV-2, where it came from, and how it is able to infect the human body. I’m going to highlight a few things from the article I thought were particularly interesting. As Cyranoski has done throughout, I’d like to stress that because this virus is so new to us and the situation is moving so quickly, many of these results are based on preliminary research, have been published in pre-print papers, and haven’t been peer-reviewed.
The first is about the detective work being done to trace where SARS-CoV-2 came from and how long it’s been in existence (possibly decades).
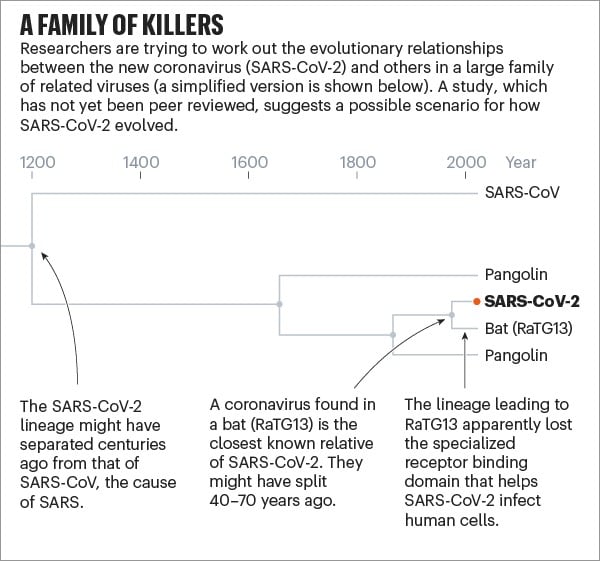
But studies released over the past few months, which have yet to be peer-reviewed, suggest that SARS-CoV-2 — or a very similar ancestor — has been hiding in some animal for decades. According to a paper posted online in March, the coronavirus lineage leading to SARS-CoV-2 split more than 140 years ago from the closely related one seen today in pangolins. Then, sometime in the past 40-70 years, the ancestors of SARS-CoV-2 separated from the bat version, which subsequently lost the effective receptor binding domain that was present in its ancestors (and remains in SARS-CoV-2). A study published on 21 April came up with very similar findings using a different dating method.
The section on how the virus acts in the body is particularly interesting because it attempts to explain the unusual and varying behaviors SARS-CoV-2 exhibits and causes in different parts of the human body. For example, SARS-CoV-2, unusually, can initially infect two places in the body: the throat and lungs.
Having these two infection points means that SARS-CoV-2 can mix the transmissibility of the common cold coronaviruses with the lethality of MERS-CoV and SARS-CoV. “It is an unfortunate and dangerous combination of this coronavirus strain,” he says.
The virus’s ability to infect and actively reproduce in the upper respiratory tract was something of a surprise, given that its close genetic relative, SARS-CoV, lacks that ability. Last month, Wendtner published results of experiments in which his team was able to culture virus from the throats of nine people with COVID-19, showing that the virus is actively reproducing and infectious there. That explains a crucial difference between the close relatives. SARS-CoV-2 can shed viral particles from the throat into saliva even before symptoms start, and these can then pass easily from person to person. SARS-CoV was much less effective at making that jump, passing only when symptoms were full-blown, making it easier to contain.
These differences have led to some confusion about the lethality of SARS-CoV-2. Some experts and media reports describe it as less deadly than SARS-CoV because it kills about 1% of the people it infects, whereas SARS-CoV killed at roughly ten times that rate. But Perlman says that’s the wrong way to look at it. SARS-CoV-2 is much better at infecting people, but many of the infections don’t progress to the lungs. “Once it gets down in the lungs, it’s probably just as deadly,” he says.
And this is a somewhat hopeful speculation on one of the many possible ways the Covid-19 pandemic could go:
“By far the most likely scenario is that the virus will continue to spread and infect most of the world population in a relatively short period of time,” says Stöhr, meaning one to two years. “Afterwards, the virus will continue to spread in the human population, likely forever.” Like the four generally mild human coronaviruses, SARS-CoV-2 would then circulate constantly and cause mainly mild upper respiratory tract infections, says Stöhr. For that reason, he adds, vaccines won’t be necessary.
Some previous studies support this argument. One showed that when people were inoculated with the common-cold coronavirus 229E, their antibody levels peaked two weeks later and were only slightly raised after a year. That did not prevent infections a year later, but subsequent infections led to few, if any, symptoms and a shorter period of viral shedding.
The OC43 coronavirus offers a model for where this pandemic might go. That virus also gives humans common colds, but genetic research from the University of Leuven in Belgium suggests that OC43 might have been a killer in the past.
But then, from a few paragraphs down:
People like to think that “the other coronaviruses were terrible and became mild”, says Perlman. “That’s an optimistic way to think about what’s going on now, but we don’t have evidence.”
For now, it’s just another thing we don’t know about this virus we learned about only 5 months ago. It’s a long road ahead, but I’m thankful that so many scientists are bent on making sense of it all.



Stay Connected